New research from Maynooth University and the Walter and Eliza Hall Institute in Australia has provided previously unachievable insight into the mechanisms behind immune response. The discovery has the potential to benefit the development of immunotherapy treatments, a promising emerging field in the fight against cancer. The research was published today in the leading international journal Nature Communications.
The research team found that in response to an infection, immune T cells develop in ‘families’ that are programmed to divide and die at different times after the infection is detected. This discovery was enabled by a new technique developed by the team that allowed them, for the first time, to follow the expansion of hundreds of individual families of cells.
The innovative method for tracking cells through generations is based on developments in division tracking fluorescent dyes. In the early 1990s, a green fluorescent dye was identified that cells can imbibe without impacting their function. When a stained cell divides, its daughters fluoresce with half the intensity of their parent, and their daughters with half again, allowing division numbers to be determined.
In the past few years, a new generation of dyes in a range of colours have been created. To enable determination of the division history of individual families, the team designed a system where each initial cell could be stained with a unique combination of colours. This allowed researchers to chart the lineages of hundreds of founding cells through multiple generations in response to a stimulating challenge.
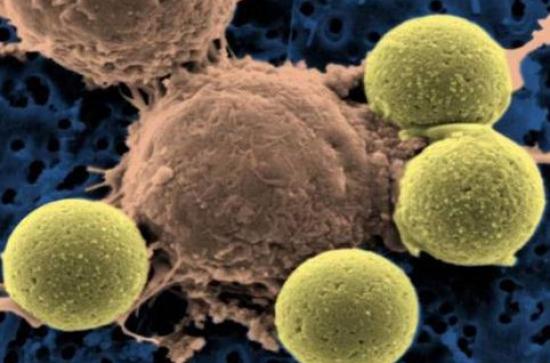
The new technique revealed how ‘families’ of immune cells develop during an immune response. Dr Julia Marchingo, who is now a postdoctoral researcher at the University of Dundee, UK, observed: “During an immune response to an infection, T cells, which recognise the invading microbe, increase in number through cell division, and become armed to fight the infection. These ‘armies’ of T cells will stop expanding at a later point, and are cleared by the death of most of the cells, leaving only a few ‘sentinels’ called memory cells that provide long lasting immunity.”
Understanding how the offspring of responding immune cells combine to provide a functioning protective response is a question of both basic scientific and practical importance. Immunotherapies are based on enhancing ineffectual immune responses by getting immune cells riled up, either by removing check-points within the body or taking fighting cells from a person, stimulating them to expand in the lab, and replanting them.
The team established that in reponse to a challenge, the T cells that respond initiate a controlled clonal programme of army building, with each cell producing a highly regimented group. They also quantitatively established how cocktails of stimulatory signals combine to produce synergistic growth.
Professor Ken Duffy, Maynooth University Hamilton Institute, said the team’s discovery was driven by an entirely new approach to analysing the immune response. “In the past we had to track immune cells using microscopy, watching individual cells over days to see whether they were dividing or dying. This was incredibly time consuming and limited our ability to understand the intricacies of the immune response. By combining laboratory techniques with mathematical analyses we could follow hundreds of T cell families, and realised that their behaviour was influenced by which family they belonged to.”
Dr Julia Marchingo, Professor Phil Hodgkin and colleagues at the Walter and Eliza Hall Institute worked with Professor Ken Duffy and Mr Giulio Prevedello from Maynooth University, Ireland, to develop this technique.
Professor Hodgkin said the research team’s discovery was an important advance in understanding how immune responses are controlled. “As well as providing new insights into how we protect ourselves from infection, this research could explain some of the problems that contribute to autoimmune disorders, when the immune system mistakenly attacks the body, as well as underpinning advances in vaccination technology,” he said.
The research was supported by the Australian National Health and Medical Research Council, Science Foundation Ireland, the European Union Seventh Framework Programme, and Australian Postgraduate Award, the Edith Moffat Scholarship, Cancer Council Victoria and the Victorian Government Operational Infrastructure Scheme.
The project was initiated when Dr Marchingo was a PhD student at the institute enrolled through The University of Melbourne’s Department of Medical Biology.
